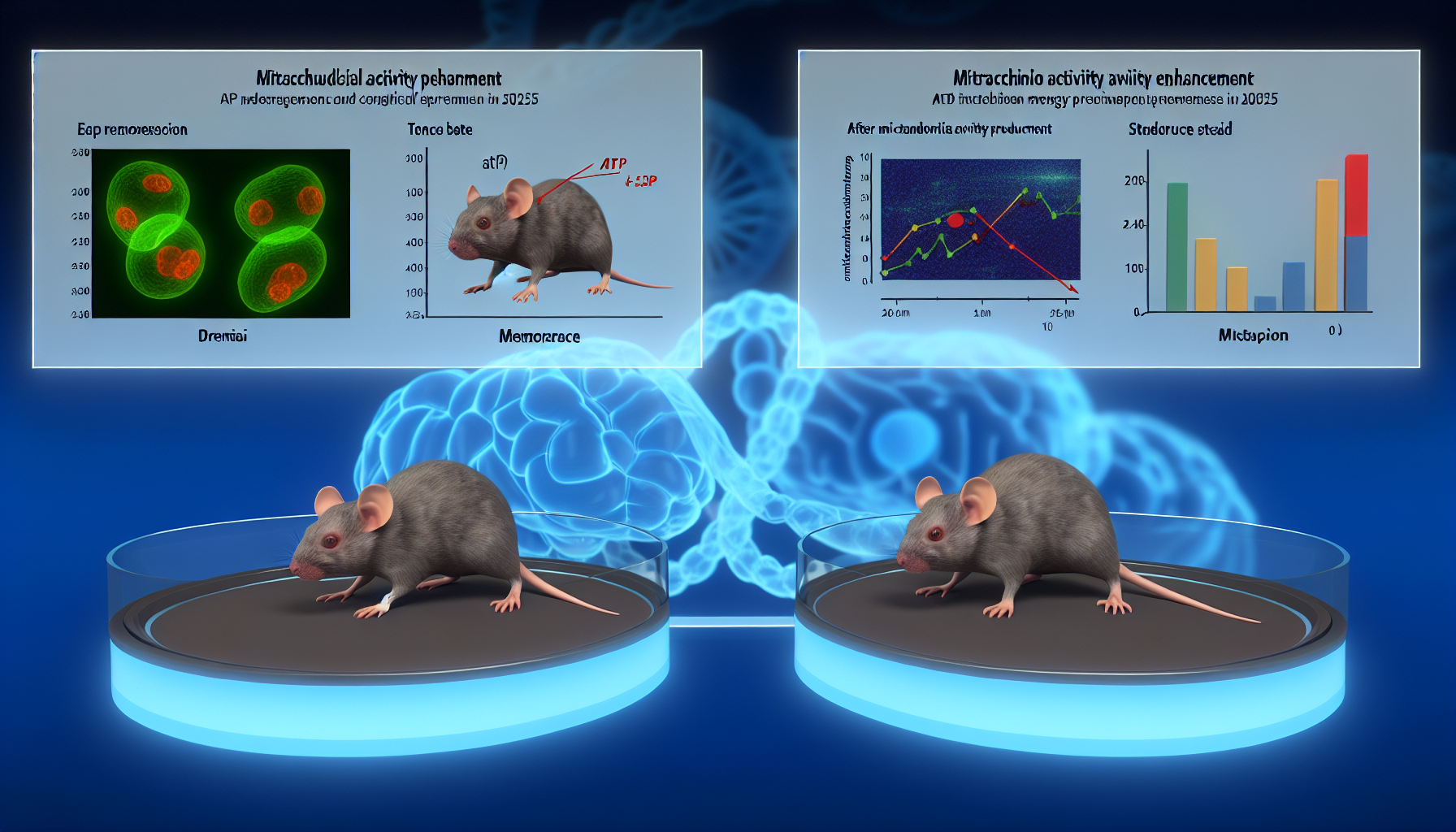
Scientists have unveiled a chemogenetic tool that directly ramps up mitochondrial activity in neurons, restores energy supply, and reverses memory loss in mouse models of dementia. The approach, tested across pharmacological and genetic paradigms, positions low mitochondrial activity not just as a correlate, but as a potential driver of cognitive decline in diseases like Alzheimer’s and frontotemporal dementia. Together with complementary 2025 data on mitochondrial DNA transcription in aging brains, the findings elevate neuroenergetics from background biology to a prime therapeutic axis.
Key Takeaways
– shows mitoDREADD‑Gs restored memory across two mouse models and normalized ATP in neurons in a 2025 Nature Neuroscience study – reveals constitutively active CREB_mito boosted mtDNA transcription in aged mice, increasing ATP reserves and improving memory in an August 2025 Science report – demonstrates INSERM (Aug 12, 2025) called this the first causal link between mitochondrial dysfunction and cognitive symptoms via a single engineered receptor – indicates Mayo Clinic (Aug 5, 2025) tied complex I disruptions to Alzheimer-like gene signatures; small‑molecule tuning of complex I activated protective programs – suggests Aug 11, 2025 plans for continuous mitochondrial stimulation will test long‑term neuronal survival and neurodegeneration delay in mouse models
How boosting mitochondrial activity restored memory in mice
The new tool—an engineered Gs-coupled receptor targeted to mitochondria and dubbed mitoDREADD‑Gs—lets researchers turn up neuronal energy production on demand. In multiple mouse models that mimic dementia-like deficits, activating the receptor normalized ATP output in brain cells and rescued performance on memory tasks. Crucially, the improvements appeared across both a pharmacological interference model and a genetic model that produces neurodegenerative phenotypes, strengthening confidence that the effect generalizes beyond a single disease mechanism [5].
ATP is the brain’s minute-to-minute energy currency. In synapses, shortfalls in ATP can throttle neurotransmission and plasticity, undermining encoding and retrieval of memories. By selectively potentiating mitochondrial activity inside neurons, the researchers effectively raised the energetic “floor” required for normal cognitive operations. That direct, cell-autonomous intervention cleanly distinguished a causal relationship: increase energy production, restore cognition. It also provides a modular platform for testing dosing schedules, brain regions, and task demands without altering nuclear genes or permanently modifying circuits.
Mitochondrial activity as a causal driver of cognitive decline
The leadership team behind the discovery underscored the shift from correlation to causation. In institutional communications, they described the work as the first causal link between mitochondrial dysfunction and cognitive symptoms, a statement anchored by controlled receptor activation that restored mitochondrial activity and behavior on demand in living animals [2]. While human translation remains ahead, that causal framing is pivotal for prioritizing targets and investment in drug discovery.
Mechanistically, the results fit a broader narrative: mitochondria sit at the crossroads of neuronal firing, calcium signaling, and metabolic flexibility. When their output dips below the threshold needed for synaptic plasticity, neurons can still fire but fail to consolidate memories. Restoring mitochondrial activity raises ATP availability, improves redox balance, and can stabilize synaptic function. The repeatable recovery across two distinct models helps rule out idiosyncratic artifacts and strengthens the case that mitochondrial underperformance is not merely a downstream epiphenomenon.
When neuronal firing boosts mitochondrial activity via mtDNA transcription
A second 2025 study in Science complements the receptor-driven strategy with a gene-expression angle. Researchers mapped an activity-dependent mitochondrial DNA transcription program—an electron transport chain “on-demand” response—and showed that enforcing it with a constitutively active mitochondrial CREB variant restored mtDNA expression, increased neuronal ATP reserves, and improved memory performance in aged mice [1]. Together, the datasets converge on a shared conclusion: in old or diseased brains, the machinery that links neuronal activity to mitochondrial output is blunted—but can be reawakened.
This activity-coupled program, sometimes abbreviated E-TC_mito, suggests a feedback loop. As neurons engage in learning, local mitochondrial gene transcription should step up to meet synaptic energy needs. With aging, that coupling loosens; neurons attempt to fire and form memories atop an energy deficit. Re-tuning the transcriptional lever (Science) or directly amplifying organelle output (Nature Neuroscience) restores the supply-demand balance. The convergence from two orthogonal methods boosts confidence that the underlying biology is robust.
Connecting mitochondrial activity to Alzheimer’s risk and treatment response
The mechanistic arc extends to Alzheimer’s disease, where mitochondrial enzymes have long been implicated. New Mayo Clinic data in 2025 tied disruptions in complex I of the electron transport chain to Alzheimer-like gene expression patterns. Using small molecules, the team quietly adjusted complex I activity and observed activation of protective cellular programs—hinting that careful tuning, rather than blunt force, could reestablish metabolic equilibrium and alter disease trajectories or treatment responsiveness [4].
These observations dovetail with the mitoDREADD‑Gs and CREB_mito results. Rather than treating mitochondria as static “batteries,” all three lines of work position them as dynamic regulators whose responsiveness to neuronal load determines cognitive outcomes. The translational promise is that multiple entry points—chemogenetic potentiation, transcriptional recoupling, or enzymatic modulation—might ultimately converge on a common therapeutic goal: stabilizing mitochondrial activity to protect and restore cognition.
What the new receptor reveals about energy and behavior
Chemogenetics, the broader framework behind mitoDREADD‑Gs, offers precision that typical small molecules cannot yet match. By targeting a Gs pathway directly within mitochondria, the method sidesteps receptor crosstalk at the cell surface and limits systemic spillover. In practice, that means cleaner tests of dose, timing, and brain-region specificity—variables that matter for memory tasks with different temporal dynamics, like object recognition versus spatial navigation.
Behaviorally, the restoration of performance implies not only enhanced energy production but likely improvements in downstream processes—ion homeostasis, maintenance of synaptic vesicle cycles, and stabilization of long-term potentiation. While the exact breakdown of contributions remains to be quantified in follow-on work, the return to near-normal behavior across two distinct models suggests the intervention targets a bottleneck common to multiple dementia etiologies.
Why mitochondrial activity matters for synapses and circuits
Neurons are uniquely energy-hungry: they maintain steep electrochemical gradients, remodel synapses with each learning bout, and shuttle organelles across long axons and dendrites. Mitochondrial activity keeps that machinery running. When demand spikes—during bursts of learning-related activity—neurons need mitochondria to ramp ATP supply instantaneously. If the ramp stalls, synapses can’t potentiate efficiently, dendritic protein synthesis lags, and the network’s ability to encode new information decays.
This is why the timing of energetic support matters. The interventions described in 2025 didn’t just raise baseline ATP; they reestablished the capacity to meet activity-driven demand. That quality—responsiveness—may be the critical determinant of whether boosting energy merely masks symptoms or actually restores the functional physiology of memory circuits.
How these findings relate to frontotemporal dementia
Frontotemporal dementia (FTD) frequently involves alterations in synaptic and metabolic genes and presents with early, profound changes in cognition and behavior. The success of a mitochondrial activity–boosting approach across both genetic and pharmacological models raises the possibility that FTD’s cognitive symptoms could also be susceptible to energy-centric therapies. Although model specifics differ from human disease, the shared endpoint—rescued memory after normalizing ATP—argues for testing mitochondrial strategies across FTD-relevant models that prioritize executive and social cognition.
As researchers refine delivery methods, they will need to consider FTD’s regional selectivity: frontal and temporal networks with high metabolic rates and unique vulnerability. Targeting those circuits with temporally precise mitochondrial support could reveal whether energy rescue translates beyond memory paradigms to decision-making, language, and social behavior—core FTD domains.
Safety, translation, and what’s next for mitochondrial activity therapeutics
No chemogenetic tool is ready for human use, but the experimental roadmap is clear. Investigators plan to test continuous mitochondrial stimulation, monitoring whether sustained energy support bolsters long-term neuronal survival and
Image generated by DALL-E 3




Leave a Reply